Physiotherapy Department
Colchester Hospital
Tel: 01206 742 530
Hip hemi-arthroplasty aftercare
This leaflet is intended as a guide for you and your family during your stay in hospital. It gives information on the operation that you have had and what to expect afterwards.
This advice is for the first six weeks after your operation.
During your stay you will be cared for by the orthopaedic team. If you or your next of kin have any questions during your stay, please do not hesitate to ask any of the ward staff.
Please be aware that your discharge planning will begin early during your stay. To assist the team in planning, please make sure that a friend or relative completes and returns the furniture height form promptly.
Average length of hospital stay is 7 to 10 days after this type of surgery.
What is a fractured neck of femur?
A fractured neck of femur is when the top of the femur, the thigh bone, is broken.
What is a hemi-arthroplasty?
A hemi-arthroplasty is the replacement of the head of the femur only, and is carried out when the socket is intact.

A metal stem is inserted inside the femur with a new ball on top, which fits inside the hip socket.
After surgery there are precautions to be followed for six weeks to avoid the risk of it dislocating.
Mobility and rehabilitation – how to care for yourself after your operation
Your mobility will be supervised by the therapy team and the nursing staff. They will teach you your bed exercises. If appropriate, you will sit in your chair on the first day after your operation. It is important to take regular pain relief for exercising and walking. Inform your nurse if you have any pain or discomfort.
Your therapist will have instructed you to put your full weight on your operated leg. You may start by using a frame and progress to crutches, if appropriate.
You will increase the walking distance daily with your walking aid, with assistance or supervision from the therapy and nursing team. This will continue until you feel confident walking without supervision. Step and stair assessments will be carried out as necessary prior to your discharge.
Physiotherapy staff will build up your exercises and you will be expected to do your exercises daily. You should continue to use your frame or crutches for six weeks after your operation or until they are no longer needed. You may be reviewed after discharge, if needed, in either your local hospital or in a community setting.
As soon as the multidisciplinary team (doctor, nurse, physiotherapist and occupational therapist) is happy with your progress, you will be discharged.
As part of your rehabilitation it is beneficial to have day clothes brought in so you can get dressed during the day. Please arrange with a relative to bring in some comfortable clothes for you and please ensure you have slippers or good fitting footwear with a solid sole and back – no flip-flops or other loose fitting footwear, please.
In some cases you may require more rehabilitation in hospital, so you may be transferred to another hospital.
Following your hip surgery
You may have heard or been taught “hip precautions” in the past. However with surgical techniques evolving and improving, research has shown that hip precautions are not always required.
Over the past few years several trusts across the UK have stopped following hip precautions with excellent results and in November 2017 Colchester Hospital adopted this practice.
We advise that you “listen to your hip” and to move as you feel comfortable to do so. If you are not following hip precautions you will be able to:
- get in and out of bed on whichever side is easiest for you
- sleep on either your back or on your side when it is comfortable to do so; and
- stop using walking aids when you are able to walk normally without a limp.
We advise that when you bend down you avoid twisting the operated leg as this could increase the risk of dislocation. The therapy team will demonstrate the correct technique with you and make sure you are happy with this.
Exercises
The exercises in this booklet are to prevent circulation problems and to improve your muscle strength and the movement in your hip. The number of times you carry out the exercises is given as a guide.
You may find you cannot manage as many to start with but you will be able to increase the number as you progress. Please remember to practice the exercises regularly because this will accelerate your progress.
It is your responsibility to complete your exercises every day. You will be shown how to do them by a member of the physiotherapy team.
Bed exercises
Breathing exercise: Take four deep breaths in through your nose and out through your mouth. Practice this every hour during the day, if possible, during the first two days.
Ankle exercise: Bend and straighten both your ankles briskly.  If you keep your knees straight during the exercise, you will stretch your calf muscles. Repeat 10 times every hour during the first few days.
If you keep your knees straight during the exercise, you will stretch your calf muscles. Repeat 10 times every hour during the first few days.
Static quadriceps: While lying on your back on your bed with your legs straight, bring your toes towards you and push your knees down into the bed. Hold for five seconds, then relax. Repeat 10 times, three times per day.

Gluteal contractions: While lying on your back, squeeze your buttocks firmly together. Hold for approximately 10 seconds, then relax. Repeat this 10 times, at least three times per day.

Abduction: While lying on your back, bring your operated leg out to the side and then back to a mid position, keeping your toes pointing upwards. Repeat this 10 times, three times per day.

Hip flexion: While lying on your back and using your operated leg, bend and straighten your hip and knee by sliding your foot up and down. Repeat this 10 times, three times per day.

Chair exercises
Foot exercise: Sit on a chair with your feet on the floor. Briskly lift both your heels off the floor and lower them. Repeat 10 times throughout the day. 
Quadriceps: Sit on a chair. Straighten your operated leg and pull your toes up towards you, tightening your thigh muscles and straightening your knee. Hold for about five seconds, then slowly relax your leg. Repeat this 10 times, three times per day. 
Knee flexion: Sit on a chair with your feet on the floor. Using your operated leg, bend and straighten your knee as far as possible. Repeat this 10 times, three times per day. 
Standing exercises
Abduction: Stand straight, holding on to a firm support. Lift your operated leg out to the side and bring it back, keeping your trunk straight throughout the exercise and your toes pointing forwards. Repeat this 10 times, three times per day. 
Extension: Stand straight, holding on to a chair. Bring your operated leg backwards, keeping your knee straight. Do not lean forwards. Repeat this 10 times, three times per day. 
Hip flexion: Stand upright, holding on to a firm support, such as a kitchen work surface or chair. Lift your operated leg up and down, bending your hip to where is comfortable. Repeat this 10 times, three times per day. 
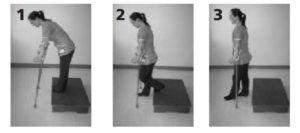
Managing stairs
Going upstairs: Place your walking aids in one hand and hold the rail with your other hand, as shown in the pictures.
- Good leg first;
- then operated leg.
- then crutches.
Going downstairs 
- Crutches first;
- then operated leg;
- then good leg.
Managing steps
Going up a step 
- Good leg first;
- then operated leg;
- then crutches.
Going down a step 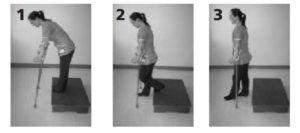
- Crutches first;
- then operated leg;
- then good leg.
Getting in and out of chairs

Getting in to bed

Getting out of bed
- Move across to the edge of the bed by bending your good leg and push up on your foot to lift your bottom.
- Shuffle your bottom around until you are sitting on the edge of the bed.
- Once sitting on the edge of the bed push up through your arms into a standing position.
Daily activities
A member of the occupational therapy team will see you in hospital to assess your ability to manage safely and independently when you return home. You may require some items of equipment, such as toileting aids and/or bed and chair raisers, which are usually loaned short term for six months.
An occupational therapist will assess your needs and arrange for a loan of equipment. The occupational therapist will work closely with your physiotherapist, nurses and doctors to help you be as independent as possible throughout the time of your recovery.
After your operation you will temporarily need to alter the way you carry out some daily activities.
The occupational therapist will make sure you feel confident with personal care tasks and teach you to use appropriate aids.
Chairs: Choose a firm, high, upright chair, preferably with arms (as they make getting up from a chair easier). Avoid sitting on a low chair. Your chair can be raised if necessary and the therapy team will advise you. Do not sit on cushions, rocking chairs, swivel chairs or chairs on wheels.
Toilet: An occupational therapist can also advise if you need any additional toileting aids. When using the toilet, do not twist around to get toilet paper and do not pull yourself up on towel rails, radiators or sinks.
Washing: Sit down to strip wash on a suitably high seat. The use of a long handled aid, such as a sponge, can be helpful.
Showering: You can get your leg wet after the clips put in during your operation have been removed and the wound is dry and healed. If you are going to use a walk-in shower, use a long handled sponge/loofah to wash the lower half of your legs and feet. Sit down on a shower stool if one is available. It is essential to use a rubber safety mat.
Important
If you feel you require an assessment of your bathing needs after discharge, please contact Essex County Council’s Adult Social Care direct (contact details at the end of this booklet).
Dressing
- Wear supportive footwear that is flat and with an enclosed back.
- Avoid tight clothing.
- Dress sitting down on a high stool, chair or bed.
- Use dressing aids, such as a long-handled shoehorn or ‘helping hand’, to dress your lower half. These can be purchased from Ableworld Mobility and Stairlifts in Colchester – 5, The Stanway Centre, Peartree Road, Colchester CO3 0JX. An occupational therapist can advise you about how to use these items while you are on the ward.
Kitchen
Try to avoid standing for long periods: If you need to stand, try to spread your weight evenly. You can stand without an aid at the sink or cooker, or use a perching stool or high seat. Re-arrange your kitchen so that the items you are most likely to use are easily accessible. You should not bend down to reach into low cupboards or a low-level oven.
Getting in and out of a car: Do not drive a car for about eight weeks after your operation, not until you can walk safely and independently across a room, and operate the foot pedals confidently. It is advisable to ask your consultant about when you can drive again. You can be a passenger in a car when you are discharged from hospital but you need to ensure the seat is high enough. It is also recommended that you sit in the front seat with the seat reclined and positioned as far back as possible.
As a passenger: The car should be parked far enough away from the kerb to enable you to get out and stand directly on the road (not the kerb). Begin with your back facing the car. Ensure you can feel the door frame against the back of your legs. Reach for the back rest of the car seat with your left hand. Put your operated leg out in front of you with the knee straight. Bend your other leg and carefully reach back for the seat base.
Lower yourself so that you sit on the edge of the seat. Using your un-operated leg, push yourself backwards on to the seat while keeping your operated leg straight out in front of you. Slowly lift both legs together into the car.
Important: Check with your insurance company and inform the Driver and Vehicle Licensing Agency (DVLA) before you return to driving in case they need to be aware of your new hip replacement.
Hobbies: It is advisable to check with your consultant before resuming physical hobbies. These general principles apply:
- Do not do any heavy work.
- Avoid excessive bending/twisting at the hip.
- Avoid periods of long standing and use a perching stool for counter-top activities.
Discharge: You will normally go home 7 to 10 days after your operation but this will depend entirely on your progress. You will be consulted fully about your discharge date. Arrangements can be made for help at home and or for further rehabilitation, as necessary. You may try general household activities at 8 to 12 weeks or at your consultant’s discretion, spreading them evenly and avoiding prolonged standing.
Advice after discharge: Stitches and clips are removed 10 to 14 days after your operation. These will be removed by a nurse at your GP surgery or on the ward if you are still in hospital.
Swelling: After surgery it is common to have swollen ankles for at least three months. To help reduce swelling, rest with your feet elevated for 1 to 2 hours every afternoon.
Exercise: Continue with your exercises at home and increase the repetitions of each exercise as you feel able to.
Slowly increase the distance you walk each day. You will probably find you tire more easily to begin with but remember you will not damage your hip by exercising. You should continue to use your frame or crutches until they are no longer needed. You may be reviewed after discharge, if needed, in either your local hospital or in a community setting.
Further information
If you have any further questions or concerns, please phone the relevant number.
- Physiotherapy Department – Tel: 01206 742 530
- Occupational Therapy Department – Tel: 01206 742 172
- Aldham Ward – Tel: 01206 742 046 or 01206 742 047
- Fordham Ward – Tel: 01206 742 042 or 01206 742 043
- Adult Social Care (Essex) – Tel: 0845 603 7630
Verifying your identity
When you attend hospital you will be asked to confirm your first and last names, date of birth, postcode and NHS number, if you know it, and to let us know if you have any allergies.
Comments, compliments or complaints about your care
Please raise any concerns in the ward or department you are in. Ask to speak with the ward sister, matron or department manager. If your concerns cannot be resolved or you wish to make a formal complaint, please look at the PALS (Patient Advice & Liaison Service) page, call PALS on 0800 783 7328 or pick up a PALS leaflet at the hospital.
Your views
If you or a family member has recently been in Colchester Hospital, you can tell us about your experience by searching for ‘Colchester’ on the NHS Choices website (Opens in a new window), by writing to us or by filling in a ‘Friends & Family Test’ questionnaire.
© East Suffolk and North Essex NHS Foundation Trust, 2021.
All rights reserved. Not to be reproduced in whole, or in part,
without the permission of the copyright owner.
Accessibility
The Recite feature on this website attempts to provide digital accessibility and translation support. If you would like to make a request for a leaflet to be produced in a different format please see our PALS contact page in order to contact the team and make a request. If you require a translation please see our translation information page. ESNEFT are actively attempting to achieve accessibility regulation compliance under the Public Sector Bodies (Websites and Mobile Applications) (No.2) Accessibility Regulations 2018.